Depression and Chronic Conditions

When first diagnosed with a chronic condition, patients often feel overwhelmed with new challenges. These might include numerous medical appointments or new prescriptions with complex dosing schedules and intimidating side effect profiles. Many patients also struggle with the unpredictable changes and functional limitations associated with their condition, the biologic effects of the disease, or a combination of these factors. Given such lifestyle changes, it is no surprise those managing chronic conditions often live with depression as well.1
Depression
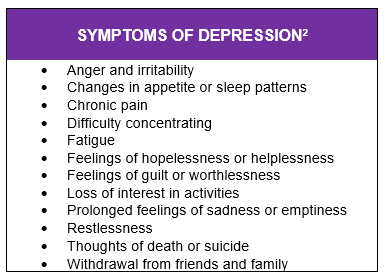
Depression is one of the most common mental disorders in the United States, affecting about 15.7 million adults. Symptoms of depression can vary from person to person (see Table below). Depending on its severity, depression can affect many aspects of daily life.
Those living with chronic medical conditions are at a higher risk for developing depression.1Research shows when a patient has a chronic disease, there is less of a chance their depression will be diagnosed.1 Some patients may mistake depression symptoms, such as fatigue and loss of appetite, with their chronic condition instead of depression.1
Identifying and treating depression is a vital part of treating chronic conditions. Understanding the links between depression and certain chronic conditions can help clinicians improve the identification, monitoring and treatment of depression in patients with lifelong conditions.
Depression in Chronic Disease
Cancer
When a patient is diagnosed with cancer, it is often an emotional time filled with uncertainties, worries and fear. Not surprisingly, depression can be common amongst cancer patients, from diagnosis throughout treatment. Although managing cancer and its treatments can be overwhelming in itself, it is also important to tend to symptoms of depression. Counseling, treatment, or certain lifestyle changes might help cancer patients manage depression and their overall health.
Chronic Inflammatory Disease
Patients with inflammatory disease, such as rheumatoid arthritis (RA) or psoriasis, also face a greater risk for depression. Depression can be the result of coping with symptoms, stigmas and disabilities resulting from an inflammatory condition. For example, patients with a visible psoriatic rash might feel isolation and embarrassment. Likewise, RA patients experiencing a flare might feel helpless when losing the ability to perform normal daily tasks. Effective management of symptoms, paired with depression screening, is critical to improving the outcomes in patients with chronic inflammatory conditions.
Multiple Sclerosis
Multiple sclerosis (MS) is a chronic, often disabling, autoimmune disease that affects about one million Americans. It is estimated that up to half of patients with MS may experience depression in their lifetime. MS can cause a wide variety of symptoms based on what part of the brain is affected. As a result, patients might suffer a number of symptoms, including fatigue, cognitive decline or difficulty completing daily tasks. It is no surprise that coping with unpredictable symptoms and a decline in functional status could lead to depression.
Transplant
Depression and anxiety are common challenges among transplant patients. Depressive symptoms have been associated with failed adherence to immunosuppressant medication. This effect is significant, as medication adherence is crucial in reducing the risk of transplant/graft failure or loss and mortality in transplant patients. Regular mental health screenings could increase a transplant patient’s quality of life and success with prescribed therapy.
Managing Depression
Learning skills to manage depression is vital to a patient’s overall well-being. Clinicians can help patients find practical ways to cope. For example, journaling might help some patients improve mental health. For other patients, staying active, engaging in activities unrelated to treatment, and socializing with others outside of their treatment community might help.3 It might also be useful for patients to define and work toward specific goals for self-care. Along with lifestyle changes for self-care, some patients might require antidepressant medication. By having open discussions about behavioral health, clinicians and patients can find the best approach to managing depression alongside a chronic condition.
Sources:
1 Simon G. Treating depression in patients with chronic disease. West J Med. 2001;175(5): 292–293.
2 Overcoming depression: how psychologists help with depressive disorders. American Psychological Association Web site. http://www.apa.org/helpcenter/depression.aspx. Published October 2016. Accessed October 12, 2020
3 Anxiety and depression. Leukemia and Lymphoma Society Web site. https://www.lls.org/treatment/managing-side-effects/anxiety-and-depression. Accessed October 13, 2020.
Back to Blog > Blog Stories




